Last Updated on October 13, 2025
How Cognitive Behavioral Therapy Helps in Treating Addiction & Prevents Relapse
At a Glance: How CBT Supports Recovery & Relapse Prevention
- What CBT does: Helps you identify the thoughts, feelings, and triggers that drive substance use, then replace them with healthier patterns.
- Core skills you learn: Self-monitoring, recognizing high-risk situations, and using practical coping strategies to manage cravings and emotions.
- Why it reduces relapse: By addressing underlying causes and teaching step-by-step behavioral changes, CBT treats relapse as a process you can anticipate and navigate—not a failure.
- Care at Nova: Offers CBT within a full continuum of services (detox, inpatient, outpatient, sober living) with an emphasis on long-term recovery.
Table of Contents
Have you heard about Cognitive Behavioral Therapy? It is one of the most important therapies for all forms of addiction. In fact, the treatment method is even useful in dealing with other psychological problems.
As the name implies, the treatment involves understanding and analyzing the behavioral patterns that are associated with addiction. For a starter, it involves observing the external and internal stimuli that are driving you towards the consumption of alcohol or any other drugs.
What Is Cognitive Behavioral Therapy (CBT)?
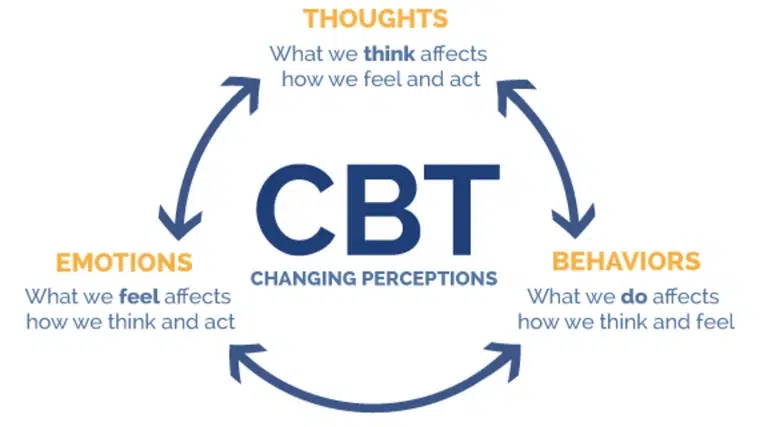
Cognitive Behavioral Therapy (CBT) is a structured, skills‑based approach that helps you see the connection between your thoughts, feelings, and behaviors. In addiction treatment, CBT aims to interrupt the cycle that links a trigger (like stress or loneliness) to a craving and then to substance use. Instead of relying on willpower alone, CBT gives you practical tools to challenge unhelpful thinking and practice healthier responses. Sessions are collaborative and goal‑oriented: you and your counselor agree on specific targets—such as reducing weekend drinking, managing anxiety without substances, or rebuilding routines—and track progress week to week. Because CBT focuses on present‑moment skills and measurable outcomes, it fits well alongside medical care and other therapeutic supports in a comprehensive addiction treatment plan. Understanding addiction as a chronic brain disease explains why ongoing skills practice matters.
How CBT Helps in Treating Addiction
Most forms of substance abuse and addiction start with casual usage and consumption. For example, social drinking sessions could have made you feel good. What started as an ordinary party with your friends and colleagues could often lead to chronic addiction.
Cognition – Trying To Understand The Underlying Cause
The underlying reason for this addiction, in this case, is the feeling of belonging that is achieved when you drink along with your friends. Slowly, your mind relates the feeling of high that is associated with drinking alcohol with the feeling of belonging. Ultimately you end up drinking in order to feel the same sense of belonging.
In CBT, you are taught how to observe and analyze the feelings, and actions that happen when you have the urge to drink or consume other substances. Once you are able to identify the cause, it becomes easier to separate yourself from the scenario and deal with the negative thoughts. CBT often works within trauma‑informed addiction treatment to reduce re‑traumatization.
Freedom Starts Here. Take Back Your Life Today.
Same-Day Admissions in Austin Available.
Behavioral Changes
You will also learn techniques and behavioral changes to cultivate to make yourself an independent individual. Practicing them in group counseling for substance abuse builds accountability. The therapy will also equip you to recognize the early signs of cravings. When you are properly trained with coping mechanisms, you will be able to successfully stay away from alcohol, marijuana, cocaine, and other habit-forming substances.
How CBT Treats Addiction Day to Day
CBT works best when it’s applied to the real situations you face. Early sessions often include a functional analysis of recent substance use: What happened right before, what you were thinking and feeling, and what happened after. From there, you’ll build a toolbox that may include:
- Trigger mapping and self‑monitoring: Spot patterns like certain people, places, times of day, or emotional states that raise your risk.
- Cognitive restructuring: Identify automatic thoughts (e.g., “I can’t handle this,” “One drink won’t matter”) and replace them with balanced, realistic alternatives.
- Skills for coping strategies for cravings: Delay, distract, and decide; urge‑surfing; paced breathing; and grounding techniques.
- Behavioral activation: Scheduling rewarding, life skills training, and substance‑free activities that boost mood and reduce boredom.
- Problem‑solving and planning: Breaking down tough tasks, setting up if‑then plans, and preparing scripts for high‑risk situations.
Over time, these skills become second nature, providing a foundation for relapse prevention long after formal treatment ends.
How CBT Helps in Prevention of Relapse
Relapse into alcoholism and addiction is a frequent event. In fact, most successful rehabilitations will have an episode of relapse once or twice. Cognitive Behavioral Therapy doesn’t see relapse as a permanent condition. Relapse is to be seen as a process of getting over your addiction. Each and everyone that undergoes treatment for addiction is under the threat of relapsing.
As CBT finds the underlying causes for all forms of addiction and it ventures into neutralizing these causes, it is effective in combating addiction. So, the probability of a long relapse is minimized.
Practices like self-monitoring, identifying high-risk situations where you will be tempted to fall back to the old ways, and understanding and combating negative emotions are all important to prevent relapse.
CBT helps you to identify such signals and respond actively to these external stimuli. It helps in
- Identification of high-risk situations.
- Maintaining emotional stability even during the flooding of emotions both negative and positive.
- Understanding the coping mechanisms.
A Walkthrough: Handling a Craving With CBT
Imagine you leave work feeling tense and lonely—two personal triggers you’ve already identified. A friend texts, “Happy hour?” Your first thought is, “I deserve it; I’ve had a rough week.” CBT invites you to press pause and run a quick skills sequence:
- Name the trigger and thought: “Stress + loneliness; thought = ‘I deserve a drink.’”
- Challenge the thought: “Deserving care doesn’t have to mean drinking. What are three other ways to unwind?”
- Choose a coping action: Text your your sponsor or peer recovery support specialist, walk for 10 minutes, then eat a balanced snack to stabilize your energy.
- Delay the decision: Set a 20‑minute timer. Cravings often peak and drop within that window.
- Decide with your values: Ask, “What choice supports my recovery tonight?” Follow through.
- Debrief: Later, jot down what worked and what to adjust next time.
Repeating this sequence builds confidence and shows you that cravings can pass—and you can steer your behavior even when emotions run high.
Relapse Prevention as a Skill Set
In CBT, relapse is understood as a process, not an event. Many people move through stages sometimes called emotional, mental, and physical relapse. By recognizing early warning signs—sleep problems, isolating, skipping meetings, idealizing past use—you can intervene sooner. A personalized relapse prevention plan typically includes:
- High‑risk situations and specific coping responses for each.
Support list: Names, numbers, and when to call. - Coping cards: Short reminders you carry or save on your phone.
- Routine anchors: Sleep, meals, activity, and connection habits that stabilize mood.
- Post‑lapse script: If a lapse occurs, steps to regain footing—contact support, re‑evaluate triggers, schedule a session—without shame or delay.
Treating relapse as information, not failure, helps you keep momentum and refine your strategy.
Core CBT Tools You’ll Practice
- Thought records: A simple table for capturing situation → thought → feeling → behavior, then generating balanced alternatives.
- Trigger/craving logs: Date, time, intensity (0–10), trigger, skill used, outcome—great for spotting patterns.
- Coping cards: Pocket‑size reminders like “Delay 20 minutes,” “Call Sam,” or “Breathe: in 4, hold 4, out 6.”
- Behavioral experiments: Test predictions (e.g., “If I skip the party, I’ll feel worse”) to gather real‑world data.
- Problem‑solving steps: Define the problem, brainstorm options, pick one, try it, review results.
- Communication skills practice: Assertive “I” statements, boundary setting, and refusal skills for social pressure.
These tools transform insights into habits, making relapse prevention concrete and actionable.
Integrating CBT With the Full Continuum of Care
No single approach fits everyone. Cognitive Behavioral Therapy for addiction is most effective when it’s integrated within a continuum of care. Many clients benefit from starting with detox (when medically appropriate), moving into residential or inpatient treatment for stability, then stepping down to Intensive Outpatient Program (IOP), sober living homes in Texas, and structured aftercare. At each stage, CBT provides consistent language and skills—so what you learn in a therapy session translates to your daily routine at home, at work, or in school. For some, combining CBT with medication‑assisted treatment (MAT) (when prescribed by a clinician) addresses cravings and withdrawal while you practice new behaviors. The continuity of skills from one level of care to the next is a powerful buffer against relapse.
Family and Support System Involvement
Recovery rarely happens in isolation. Involving family or trusted supports in select CBT sessions can reduce misunderstandings, build healthier communication, and align expectations. You might practice boundary setting (“I’m not attending events at bars right now”), request specific support (“Please check in with me after work on Thursdays”), or co‑create plans for handling triggers at home. Loved ones also learn to distinguish support from enabling, which protects your progress and strengthens the household’s resilience.
Measuring Progress and Staying Motivated
CBT values evidence—your own evidence. Together with your counselor, you’ll set measurable goals: number of sober days, craving intensity, sleep quality, or participation in recovery activities. Each week you review what’s improving, where you’re stuck, and which skills to tweak. Many clients use visual trackers or brief check‑ins to keep motivation high. Celebrating small wins matters: finishing a stressful week without using, handling a conflict with new communication skills, or attending all scheduled sessions are clear signs that addiction treatment is working. If progress plateaus, the plan can be adjusted—more support, different skills, or coordination with medical providers.
What to Expect in Your First Sessions
Early sessions focus on assessment and goals. You’ll discuss substance use history, strengths, current stressors, and what you want from treatment. Your counselor will explain how CBT works and help you identify a few high‑impact targets—for example, “Reduce after‑work cravings,” or “Handle family conflict without drinking.” You’ll leave with one or two simple practices (like tracking triggers or using a breathing exercise) and a plan for the week. As therapy continues, you’ll refine your relapse prevention plan, build confidence through real‑life wins, and connect with the right level of care—whether that’s residential treatment, outpatient sessions, sober living, or ongoing aftercare.
Where Do I Turn For Help?
At Nova Recovery Center, we provide the best cognitive behavioral therapy to combat your addictions. It trains you mentally, emotionally, and physically to stay out of substance abuse. We have many sober living homes and detox centers Austin in Texas. Book an appointment today. If you feel that you need help with an addiction and want to learn more about outpatient drug rehab in Austin, Texas, please call Nova Recovery Center at (888) 427-4932 or contact us online today.
Frequently Asked Questions About CBT for Addiction, Treatment Options, and Relapse Prevention
What is cognitive behavioral therapy (CBT)?
CBT is a structured, short‑term form of talk therapy that helps you identify and change unhelpful thoughts and behaviors; it’s often used alone or alongside medications and is also used for substance use disorders. CBT is also first‑line for behavioral addictions.
How does CBT help with addiction?
CBT teaches practical skills—like spotting high‑risk situations, challenging automatic thoughts, and using coping strategies—to reduce substance use. It has demonstrated efficacy as a stand‑alone treatment and as part of combination approaches.
Is CBT effective for substance use disorders (SUDs)?
Evidence from large trials and meta‑analyses shows CBT produces meaningful improvements for alcohol and drug use disorders, with effects comparable to other active treatments.
What techniques are used in CBT for addiction?
Common elements include self‑monitoring (tracking triggers/cravings), cognitive restructuring, problem‑solving, skills training, and relapse‑prevention planning and other specialized therapies as needed.
How long does CBT usually take?
CBT is typically delivered in a limited number of structured sessions and may include between‑session “homework” to practice skills.
Can CBT help prevent relapse?
Yes. Relapse prevention is a core CBT application: skills development, medications when indicated, monitoring, and social support all reduce risk over time.
What are the stages of relapse?
Many programs describe relapse as a process with stages—often emotional, mental, and physical relapse—allowing earlier recognition and intervention.
What are common relapse triggers?
Risk factors include the severity of addiction, co‑occurring conditions, and gaps in coping skills/support. Internal states (stress, strong emotions) and external cues (people/places) can trigger cravings.
What is medication‑assisted treatment (MAT), and can it be combined with CBT?
MAT uses FDA‑approved medications (e.g., buprenorphine, methadone, naltrexone for OUD; naltrexone, acamprosate, disulfiram for AUD) with counseling/behavioral therapies like CBT—a whole‑patient, evidence‑based approach.
How long does addiction treatment last?
Duration varies by substance, severity, and setting; treatment is best viewed like other chronic conditions—ongoing care and periodic adjustments support long‑term recovery. Learn more about how long drug rehab is.
Is relapse a normal part of recovery?
Relapse does not mean treatment or recovery has failed. Like other chronic illnesses, it signals the need to resume, modify, or change treatment.
Other Drug and Alcohol Rehab Locations
Medical Disclaimer
The information on this page is provided for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Cognitive Behavioral Therapy (CBT) and other therapeutic approaches should only be practiced under the guidance of a qualified mental health professional. If you are struggling with substance use, experiencing withdrawal symptoms, or are in crisis, seek immediate medical attention or call 911 in the United States.
Nova Recovery Center Editorial Guidelines
By instituting a policy, we create a standardized approach to how we create, verify, and distribute all content and resources we produce. An editorial policy helps us ensure that any material our writing and clinical team create, both online and in print, meets or exceeds our standards of integrity and accuracy. Our goal is to demonstrate our commitment to education and patient support by creating valuable resources within our realm of expertise, verifying them for accuracy, and providing relevant, respectful, and insightful data to our clients and families.
- American Psychological Association. (n.d.). Cognitive behavior therapy (CBT). APA Dictionary of Psychology. https://dictionary.apa.org/cognitive-behavior-therapy (Accessed October 13, 2025).
- Guenzel, N., & McChargue, D. (2023). Addiction relapse prevention. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551500/ (Accessed October 13, 2025).
- McHugh, R. K., Hearon, B. A., & Otto, M. W. (2010). Cognitive behavioral therapy for substance use disorders.Psychiatric Clinics of North America, 33(3), 511–525. https://pmc.ncbi.nlm.nih.gov/articles/PMC2897895/ (Accessed October 13, 2025).
- National Institute on Drug Abuse. (2025, June 9). Treatment. https://nida.nih.gov/research-topics/treatment (Accessed October 13, 2025).
- Substance Abuse and Mental Health Services Administration. (n.d.). Evidence‑Based Practices Resource Center.https://www.samhsa.gov/libraries/evidence-based-practices-resource-center (Accessed October 13, 2025).